Myopia - An Overview
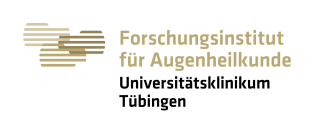
During normal postnatal eye development, refractive errors that may be present in early infancy disappear, resulting in "emmetropia" and optimal visual distance acuity at around the age of 5.
The process ("emmetropization") occurs by matching the length of the eye to the focal length of the cornea and crystalline lens with an impressive precision (about 100µm in axial length of the eye, which is much less than 1% of the length of the eye of 24 mm). In an emmetropic eye, far objects are focused on the retina when accommodation is relaxed.
As a result, the accommodation amplitude (active changes in the focal length of the lens, controlled by the ciliary muscle) is available to focus from infinity to close (see also Adrian Glasser).
In the industrial nations, the eyes tend to become too long (although emmetropization seems initially successful, since refractive errors are rare around five years of age). This condition, where the plane of the sharp image is in front of the retina, is called "myopia" (or nearsightedness).
Even with relaxed accommodation, distant objects can no longer be focussed. Myopia can be optically corrected by spectacles, contact lenses or re-shaping the cornea by refractive surgery, which is done by laser ablation.
Although optical correction is often mainly a cosmetic problem, the fact that myopia is getting more frequent, develops earlier and reaches higher end point refractions goes along with an increased risk of later blindness due to retinal detachment, retinal degeneration, glaucoma and cataract. The average frequency of myopia in young adults reaches about 30% in the western industrial nations but can reach more than 80% in the asian countries.
Overview articles can be found here (in German, Adobe PDF document, 720 kByte, © by Springer-Verlag GmbH & Co.KG)
and in English from "Essentials in Ophthalmology" (ed. by Krieglstein GK and Weinreb RN), volume "Pediatric Ophthalmology, Neuro-Ophthalmology, Genetics" (ed. Lorenz B and Moore AT), pp 1-18 (Springer Verlag, Heidelberg) here (Adobe PDF document, 630 kByte).
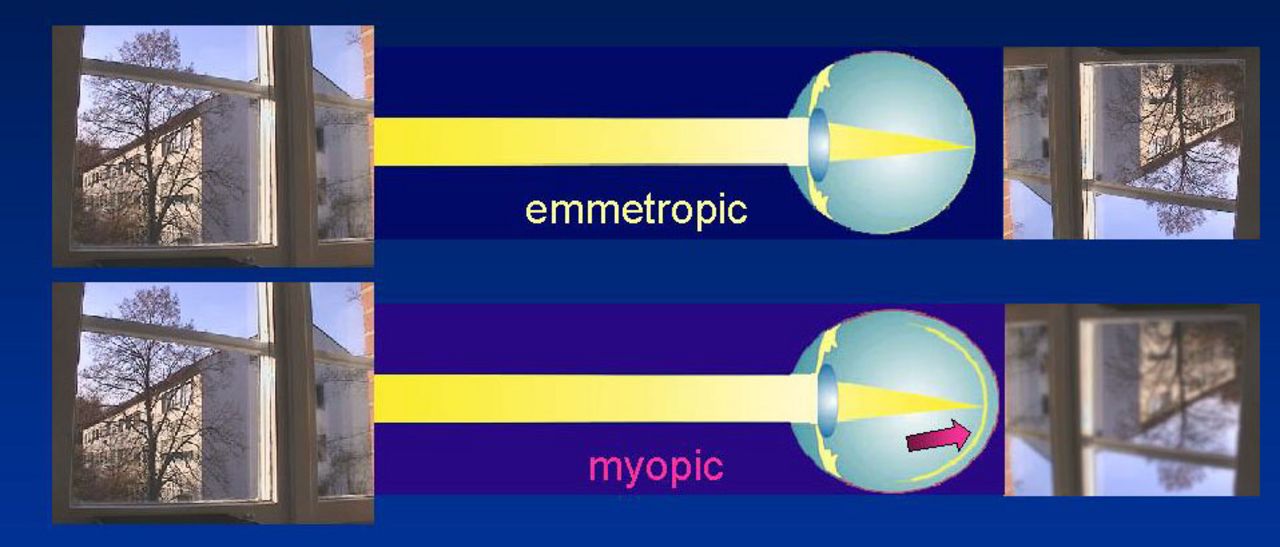
There is no causal therapy for myopia, because its mechanisms are still not well understood. Our laboratory studies both the visual and genetic control of eye growth in two animal models, the chicken and the mouse, and in humans.
We use several different technological approaches:
- optical - psychophysical - F. Schaeffel, J. Tabernero, A. Ohlendorf, T. Tepelus;
- immunohistochemical - E. Burkhardt, U. Mathis;
- molecular biology - M. Feldkämper, R. Schippert , A. Penha, R. Ashby;
- electrophysiological - E. Diedrich, F. Schaeffel.
Key contribution to myopia research
A key contribution to myopia research, together with Adrian Glasser and Howard C. Howland was our first demonstration that the growth of the eye can be predictably altered by spectacle lenses (picture from Vision Research 1988).
Worldwide, there are currently about 25 laboratories which study the mechanisms of myopia in chickens, marmosets, tree shrews, rhesus monkeys, guinea pigs and humans.
Every two years, people meet at the "International Conference on Myopia", this time in Cairns Australia (about 300-500 participants).
In addition, at the Annual meeting of the "Association for Research in Vision and Ophthalmology, ARVO in Ft. Lauderdale, Florida, most of the myopia researchers are also present and discuss their results with a larger vision research community (in total about 8000 participants).
In the photographs below: Chick treated unilaterally with a -7D lens bzw. chicks treated unilaterally with a -7D lens
Are there drugs against myopia and where can I get them?
(a) Atropine, a relatively unspecific muscarinic antagonist, has been found effective against myopia development in children (literature for example: Shih et al, 2001; see medline, look for "shih" and "atropine"). However, it paralyzes accommodation (no focus for close objects, reading glasses necessary) and its mode of action is complex (at least 5 targets of action). Used in the far East, rarely in Europe or USA.
The effect of atropine on myopia has recently been more extensively examined in the "Atropine in the Treatment of Myopia" ("ATOM") study (Singapore) in which initially 400 myopic children (refractions -1 to -6D) were randomly assigned to either 1% atropine eye drops, given unilaterally every evening, or to placebo treatment.
After one year, the myopia progression in the placebo-treated eyes was -0.76 D ± 0.44 D but in the atropine-treated eyes there was a regression of myopia by +0.3 D ± 0.50 D (difference p < 0.0001). Axial length increased by +0.20 mm ± 0.30 mm and even regressed by -0.14 mm ± 0.28 mm (p < 0.0001), respectively.
After 2 years, the increase in myopia was -1.20 D ± 0.69 D, versus -0.25D ± 0.92 D in the atropine treated eyes.
At a special interest group meeting at ARVO 2004, it was shown that, after 24 months, myopia started to progress also in the atropine treated eyes, so that the largest difference between atropine and vehicle treatment occurred probably at 1.5 -2 years.
This study also showed that younger kids are more sensitive to atropine treatment, and that slowly progressing myopes showed better effects.
Generally, it looks as if the eyes adapt to atropine treatment so that the effects on myopia wear out. The assumption receives support from the observation that the pupils appear no longer fully dilated after 2 years of continuous atropine treatment.
(b) Pirenzepine has been claimed to reduce myopia progression in children by about 50% (= 0.26D less myopia progression in 12 months, 117 children with Pirenzepine 2%, 57 with placebo, ages 8-12 years; Siatkowski et al, ARVO 2003, Poster #4778).
However, similar to atropine, the effects of pirenzepine on myopia progression occur mostly in the first year of treatment. In addition, pirenzepine is generally less potent and, to achieve a significant effect, a 6mm strip of pirenzepine gel (2%) had to be placed in the cul de sac every evening.
Subconjunctival injections of Pirenzepine in rhesus monkeys have shown (ARVO 2004, #1745, see "abstractsonline.com", search for "Glasser") that significant reductions of accommodation amplitudes and pupil responses occur already with a 0.02% concentration of the injected solution, suggesting that pirenzepine is no longer M1 receptor-specific even at this low dose. At a concentration of 2%, as used in myopia treatment, it is likely that Pirenzepine binds to all muscarinic and probably also to other receptors.
The patent for Pirenzepine treatment of myopia was licensed by Novartis at the begin of 2003.
However, it was returned to ValleyForge at the end of the year, perhaps because the data from the second year of the trial were less convincing than expected.
Currently, it is no longer so clear whether Pirenzepine will become commercially available in the near future as an accompanying therapy for myopia in children. Also, the mechanisms by which Pirenzepine exerts its effects on myopia are still poorly understood, and there are almost no data on its effects on retinal function.
Since Pirenzepine did not show reliable effects on myopia progression after extended application, the phase III clinical study was not undertaken and it will not be marketed.
(c) Glucagon: selective agent against deprivation and lens induced myopia in chickens.
Even more powerful than glucagon itself was Oxyntomodulin, also a glucagon-related peptide (Vessey, Rushford and Stell, ARVO 2004, #1231; see "abstractsonline.com", search for "Stell").
The retinal glucagon pathway seems to be a promising target for pharmacological intervention. However, glucagon could not be detected in the retina of mammals. It is necessary to uncover the peptides that have taken over its function in emmetropization.
No data yet from other vertebrates.
(d) Dopamine agonists have regained some interest recently. However, they require extensive studies on possible changes in visual function.
What other possibilities are there to reduce myopia progression?
(a) There are human data suggesting that a "good" reading distance (30 cm or more) is important; (see medline, look for "Parssinen" and "Lyyra", 1993).
(b) In chickens, there is some evidence that poor illumination can increase myopia development; (see medline, look for "Feldkaemper M.", 1999).
(c) There are a number of studies suggesting that reading glasses (plus lenses) may be beneficial.
However, the biggest effects were found in the far East; (see medline, look for "Leung J.T." and "Brown B.").
Less was found in the US; (see medline, look for "Fulk G.", 2000). It is not clear at present whether reading glasses should be prescribed to children with progressing myopia (see also the COMET study).
The results of the COMET study were disclosed in the April issue of Investigative Ophthalmology and Visual Science, the highest impact journal in Ophthalmology
The results are: similar to previous studies, progressive addition lense reduced the myopia progression a little bit (although this was statistically highly significant). (fig.4)
However, the authors consider the effect as "clinically not significant". This means, there is no justification to prescribe reading glasses to children with progressing myopia because the effect is only 14% reduction. Even after 3 years with reading glasses, the difference between the children with normal spectacles and with reading glasses was only about 0.2D.
Nevertheless, the COMET study shows convincingly that the spectacles have a significant effect on refractive development also in humans. This was proposed based on results form animal models already in 1988.
At ARVO 2004, it was shown which subset of children in the COMET study responded best to the treatment with progressive addition lenses (PAL). In children with (1) near esophoria (eyes more crossed during reading), (2) lag of accommodation more than 0.43 D (=more than the total group average), (3) less myopia than -2.25 (which were also the slower progressors), the PALs were actually quite effective, with an average reduction in myopia progression by about 50% (Jane Gwiazda, Boston). The best age for starting the treatment is 8 to 9 years (Leslie Hyman, Director, COMET coordination center). This indicates that a kid should be selected for treatment based on the criteria listed above.
(d) There is also some evidence that hard contact lenses may reduce myopia progression in children (see medline; enter "RGP lenses myopia"), although not in all cases.
Currently, the "Contact lens and myopia progression" study (CLAMP study) is underway in the USA to finally clarify this question (Jeff Walline, Columbus, Ohio).
The outcome of a major study on the effect of hard contact lenses on myopia progression was not very convinving, which made the authors conclude that "RGPs (rigid gas permeable contact lenses) should not be prescribed primarily for myopia control":
Walline JJ, Jones LA, Mutti DO, Zadnik K.
A randomized trial of the effects of rigid contact lenses on myopia progression.
Arch Ophthalmol. 2004 Dec;122(12):1760-6
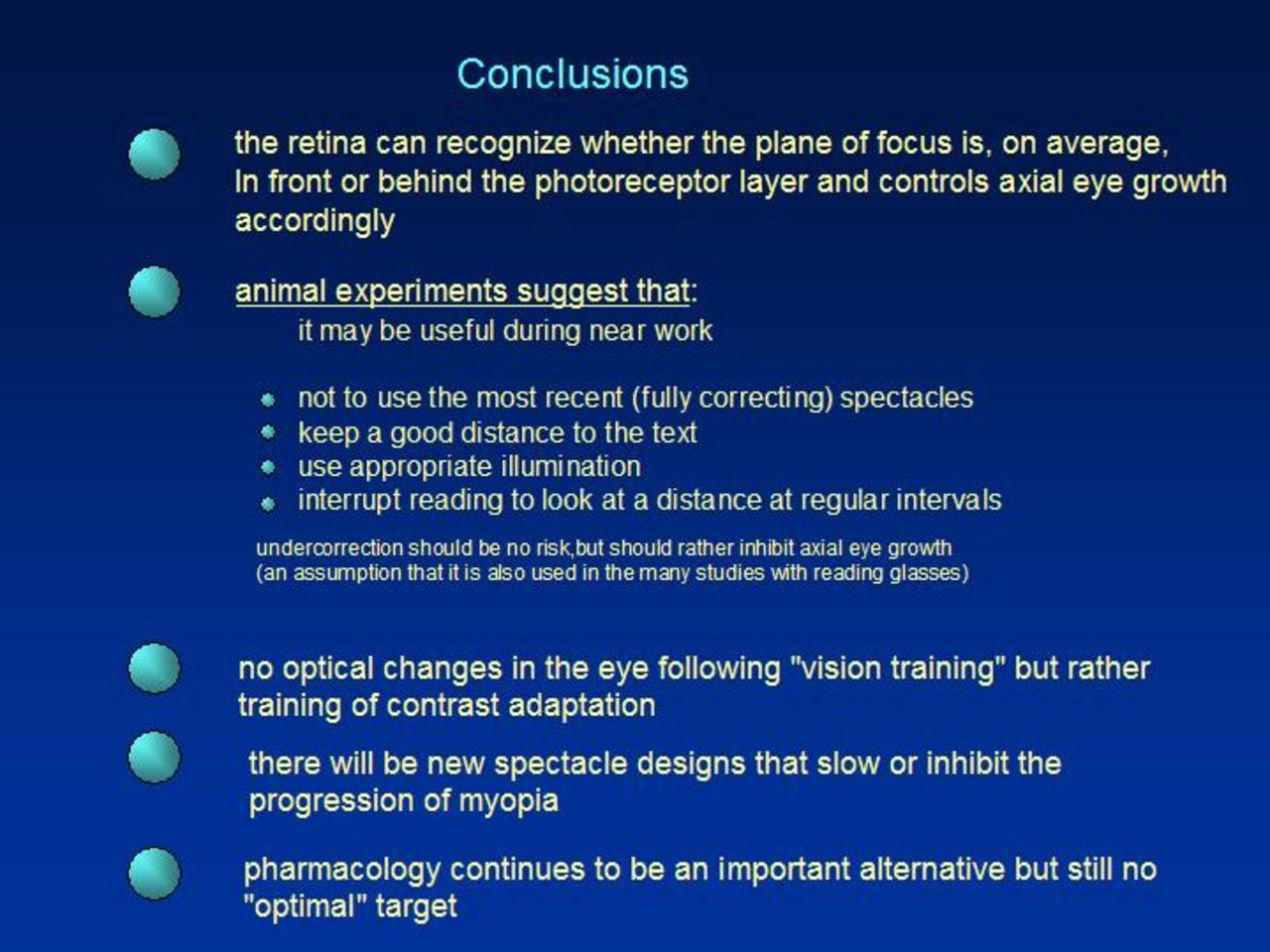
(e) Results from animal models show that much less myopia is induced if the treatment with negative lenses or frosted occluders is interrupted for only a few minutes; (see medline, look for "Smith E., myopia", and "Wallman J., myopia").
It is possible that also short periods of interruption of reading and looking at a distance may be an effective way to reduce myopia progression.
It is also interesting that defocus imposed by positive lenses (focussed image in front of the retina) is extremely powerful to inhibit axail eye growth in animal models. Four times of positive lenses wear for only 2 minutes per day can completely suppress myopia development that woould otherwise be induced by negative lenses, worn for the remaining part of the day.
At ARVO 2004, the laboratory of Josh Wallman, New York, presented data showing that the signal for inhibition of axial eye growth is generated by positive lenses in only 2 minutes (Zhu, Liu, Ganiez and Wallman, ARVO 2004, # 4285) ... does this mean that 2 minutes of interruption of reading would be sufficient to inhibit reading-induced myopia also in humans? (see abstractsonline.com, search for "Wallman")
(f) The results of the animal experiments suggest that myopia correction by spectacles should be done hesitating (although it is clear the good correction is necessary for driving and in lectures or school). Low myopes could read without glasses and higher myopes with their previous spectacle corrections, to reduce the lag of accommodation.
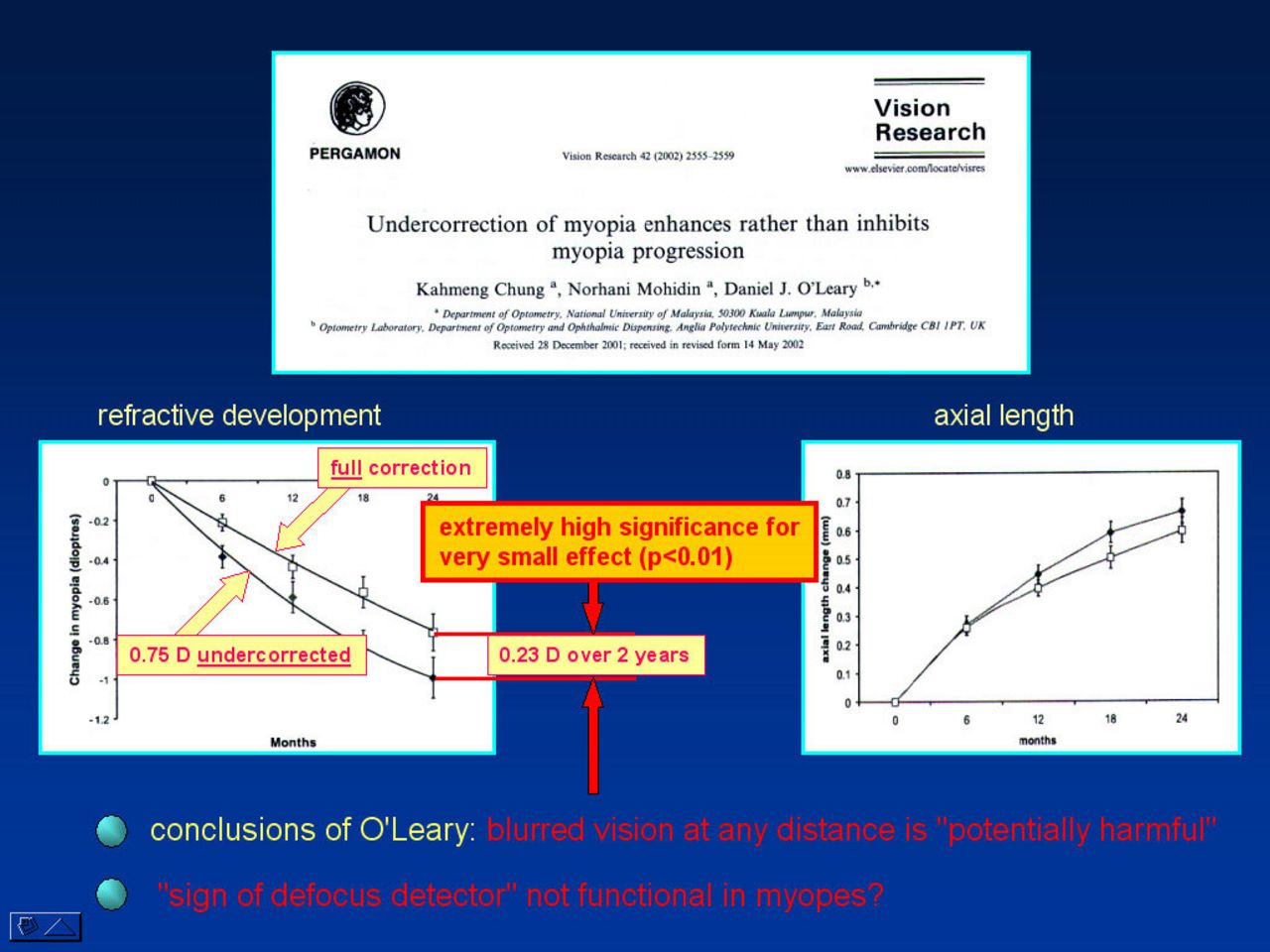
Since full correction at all viewing distances is assumed to promote the progression of myopia in children, it has been common to correct myopia not fully but perhaps a quarter of a diopter below perfect distance correction.
This practice was challenged by a recent study by Chung et al (Vision Research 2002) which attracted considerable attention in the public media. It was claimed that the "wrong" (under) correction would result in faster, rather than slower, myopia progression and that the correction scheme should be revised. (fig. 6)
However, one should not ignore the magnitude of the effect. Given that the undercorrection was quite severe (0.75D), the difference in refraction in both groups was only 0.23D in two years (which was statistically surprisingly significant, given that the relatively small group sizes of about 45). It may be necessary to wait for the results of more studies from Europe or the US before the current correction strategy is changed.
A summary of the different attempts to inhibit myopia progression is shown in the picture below (re-plotted after Dr. Wei-Han Chua, presented at ARVO 2004).
A summary of the different attempts to inhibit myopia progression is shown in the two pictures fig. 7, fig. 8, (re-plotted after Dr. Wei-Han Chua, presented at ARVO 2004).
The first shows the effects on myopia development after 1 year of treatment, the second after two years of treatment. Note that atropine in the first year is by far the most powerful intervention. Note also that the effect of undercorrection is small despite its surprising significance, given the relatively low number of subjects.
How important is the genetic background?
It may be quite important, perhaps more than the animal experiments suggest. It is disturbing that none of the animals would have become myopic without lens or occluder treatment. Yet, a number of kids become myopic even though their visual experience is not very different from other kids who remain emmetropic. As long as we don't know how important the visual input is in myopia in humans, it can also not be determined, how effective suggestions a - f in (2) are. If the genetic background is the major factor, treatment with drugs may be the major way to go. Unfortunately, reading and near work cannot be reduced much.
At ARVO 2004, a number of attempts were presented to identify genes that may be responsible for myopia development (see abstractsonline.com, search for "myopia").
Does reading at low light increase the risk of myopia in children?
Although there are no studies available from monkeys or humans, showing that reading at low light can promote myopia development, there are some hints from experiments with chickens (fig. 9).
Based on these data, it could be concluded that there may be some risk that low light can cause more myopia, although it is not as efficient as poor image contrast and low pass filtering - see myopia with the diffusers in Figure 9.
Published in Experimental Eye Research 1999:
Feldkaemper M., Diether S., Kleine G., Schaeffel F.
Interactions of spatial and luminance information in the retina of chickens during myopia development
Exp Eye Res. 1999 Jan;68(1):105-15)
What is the influence of the environment on myopia development?
There are many data suggesting that myopia has a major genetic component. This can be seen, for instance, in the high correlations of the refraction in twins (about 90 percent), but also in the fact that myopic parents often have myopic children (roughly 10 percent chance of myopia with no myopia in the parents, 30 with one myopic parent and 60 with both parents myopic). In populations where everybody has similar visual experience or a similar environment, genetics determines refractive development to a large extend.
However, if individuals originating from one population have diverse visual or environmental exposure, the effects of environment show up very clearly.
This fact have all nicely been described in a review by Ian Morgan and Kathy Rose in 2005, which was, among others, discussed in the New Scientist (Fig. 10).
Are there new optical techniques to interfere with myopia development?
Since it has been shown by the laboratory of Earl Smith in Houston that refractive errors can be induced in monkey just by changing the focus in the periphery of the retina, people realized that the peripheral refractive error with spectacle lenses may be important also in humans. Several attempts are currently made to generate spectacle lenses that impose some myopic refractive error in the periphery while keeping the fovea in focus.
In the frame of our RTN "MyEuropia", we are testing the effects of such new lenses on visual performance and peripheral refractive errors. In the future, we will test extensively how the natural refractive errors are in the periphery of the visual field in children. Finally, studies are planned in which the effects of the traditional spectacles on myopia progression are compared to the effects of newly designed ones.
(answers may be biased by the personal views in the Section of Neurobiology of the Eye)