DFG-SPP2127 - “Gene and cell based therapies to counteract neuroretinal degeneration”
| Project 1: | Selecting the right patients for gene-based therapies: Development and implementation of a pathogenicity scoring system combined with functional in vitro and in vivo validation of gene variants and genotypes in patients with inherited retinal dystrophies as a criterium for the eligibility for therapeutic studies |
|---|---|
| Principle Investigator: | Susanne Kohl |
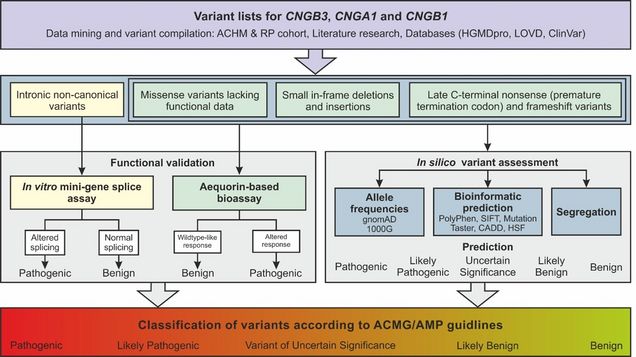
The number of gene therapy trials for inherited retinal dystrophies is steadily increasing. It is important to ensure that the disease in these patients is truly and exclusively caused by the mutations in the target gene of gene therapy. Current practice for selecting patients for gene therapy in terms of genotype or its validity is neither objective nor standardised. Guidelines for variant interpretation in genetic diagnostics need to be further developed and standardised on a subject-specific basis. An objective and reliable pathogenicity assessment for individual variants and patient genotypes needs to be undertaken as an essential criterion for selecting patients into genotype-based therapy trials. In the first funding period, we correlated the scoring system for individual variants and patient genotypes as a proof-of-concept with functional data from our further developed in vitro aequorin-based bioassay for functional testing of missense variants in CNGA3. In the sequel application, we will first transfer this bioassay to CNGB3, and then to CNGA1 and CNGB1. We will again test the functionality of CNG channels with all previously uncharacterised putative disease-causing missense variants in a medium-throughput format in HEK293 cells. With this approach, we can evaluate all non-functionally characterised variants and confirm or reject the in silico prediction. At the end of the SPP, we expect to have an objective functionally confirmed pathogenicity assessment for all CNGA3, CNGB3, CNGA1 and CNGB1 variants observed in our patient cohort, literature and various mutation databases. This will allow patients to be prioritized and selected for future gene therapy trials for autosomal recessive achromatopsia – in the case of biallelic mutations in CNGA3 or CNGB3, and autosomal recessive Retinitis pigmentosa – in the case of biallelic mutations in CNGA1 or CNGB1.
| Project 2: | CRISPR/Enhanced-Deletion Cas9-mediated allele-specific targeting of the rhodopsin gene: a novel mutation-independent approach to treat RHO-linked autosomal dominant Retinitis pigmentosa |
|---|---|
| Principle Investigator: | Bernd Wissinger |
Inherited retinal dystrophies (IRD) are a heterogeneous group of genetic disorders with an estimated prevalence of 1 in 3,000-4,000 individuals. Retinitis pigmentosa (RP) is the most common subform of IRD and characterized by night blindness and progressive degeneration of rod photoreceptors which leads to loss of peripheral vision, and eventually blindness in advanced stages. In our large local cohort, dominant inherited RP (adRP) accounts for 11.5% of all IRDs. Mutations in RHO encoding the apo-protein of the rod photoreceptor visual pigment is the most common cause of adRP. The Human Genome Mutation Database lists 247 likely disease-causing RHO variants, the vast majority (>200) being missense variants associated with adRP. Since dominant RHO mutations typically act as gain-of-function or dominant-negative mutations, we propose to apply a novel bioengineered CRISPR/Cas genome editing variant to selectively disrupt RHO mutant alleles mutation-independently, while preserving the integrity of wild-type allele. Specifically, different frequent heterozygous SNPs in cis with the specific mutations are targeted to disrupt the activity of mutant RHO. On the whole, the cumulative frequency of the selected SNPs is estimated to be present in >40% of the patient population, enabling to address a large subcohort of RHO-adRP cases. Considering future in vivo application and clinical translation potential of this approach, we will employ novel bioengineered CRISPR/Cas variants that are amenable for delivery via recombinant AAV vectors. Patient-derived cellular models will be implemented for the assessment and validation of the proposed mutation-independent genome editing approach.
These projects are part of the DFG-SPP 2127: Gene and cell based therapies to counteract neuroretinal degeneration (https://www.spp2127.de/) aiming to find effective ways to treat rare eye diseases.
DFG-Schwerpunktprogramm SPP 2127: Gen- und Zellbasierte Therapien für die Behandlung neuroretinaler Degeneration (Projekt Nr. 360003551) gepris.dfg.de/gepris/projekt/360003551 | |
Project Coordinator: | Knut Stieger, Klinik und Poliklinik für Augenheilkunde, Universitätsklinikum JLU Gießen, Friedrichstraße 18, 35392 Gießen |
| Second Funding Period |
|
Other Partners: |
|
First Funding Period |
|
Funding Agency: | Deutsche Forschungsgemeinschaft (DFG) |